This blog has been medically reviewed by Theresa Vuskovich, DMD.
Sleep is the perfect time to wind down after a long day, but if a snoring partner is keeping you awake, it can turn midnight hours into a nightmare instead of a dream. Late at night, it’s easy to slip into a helpless mindset: “I think my partner has sleep apnea, but how can I tell?”
Snoring partners may be more common than you expect. A survey from the National Sleep Foundation found that nearly one in four couples sleep in separate beds. Along those lines, snoring affects about 57 percent of men and 40 percent of women. No wonder so many couples are struggling to sleep through the nighttime rumblings of their partner!
It’s easy to understand why many couples choose not to cuddle up next to each other every night when you consider the harmful effects of losing sleep. People aren’t just waking up tired due to late-night snoring from their partners. Lack of sleep is also impacting their overall mental and physical health, building resentment in their relationship, and affecting their ability to function at work.
Plus, on top of the personal struggles an individual can experience with a snoring partner is the worry that the snoring is a sign of something even more serious. We’re here to help break down how to tell if your partner has sleep apnea and give you the information you need to make the best decision for you and your partner’s health.
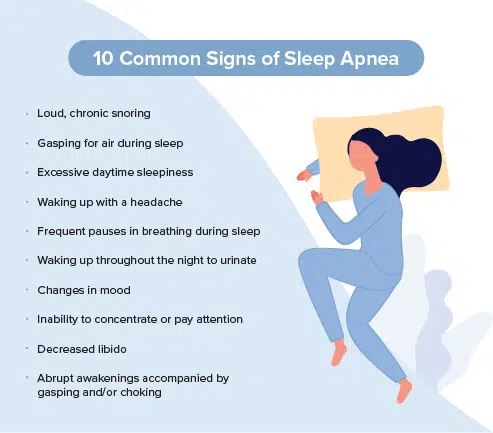
Common Symptoms of Sleep Apnea to Look for
(That You’ve Probably Already Noticed)
It can be difficult for people with sleep apnea to realize they have it. In fact, an estimated 80 percent of people with obstructive sleep apnea (OSA) remain undiagnosed despite access to health care. Luckily, partners are often able to notice the most common signs and symptoms of sleep apnea.
If you’ve ever said to yourself, “I think my husband has sleep apnea,” while lying awake at night, it was probably while noticing some of the most common signs of the disorder, including the following:
- Loud chronic snoring
- Frequent pauses in breathing during sleep
- Gasping for air during sleep
- Waking up throughout the night to urinate
- Excessive daytime sleepiness
- Waking up with a headache
- Changes in mood
- Inability to concentrate or pay attention
- Decreased libido
- Abrupt awakenings accompanied by gasping and/or choking
At this point, you may be thinking to yourself, “My partner has sleep apnea.” If this thought is running through your head, it’s absolutely essential to reach out to a doctor for more information.
The Risks of Untreated Sleep Apnea
Not only can sleep apnea result in debilitating everyday symptoms such as fatigue, difficulty concentrating, and irritability, but it is also associated with serious, chronic health concerns.
Conditions That Can Occur
If you think your wife or husband has sleep apnea, it’s essential to realize that obstructive sleep apnea is a serious medical condition. The following are just a few of the complications associated with OSA:
Cardiovascular Disease
OSA has been linked to many forms of heart disease, including hypertension, arrhythmias, coronary artery disease, and stroke. Studies have found that individuals with severe sleep apnea are at an increased risk of these diseases independent of risk markers or demographics, which means anyone with OSA could be more likely to develop or exacerbate these conditions.
Diabetes
Current evidence suggests type 2 diabetes is more prevalent among patients with OSA compared to those without OSA, independent of shared risk factors.
According to frontiers in Neurology, up to 83 percent of patients with type 2 diabetes may be suffering from undiagnosed OSA. The severity of OSA is also associated with the worsening of glucose control overall.
Alzheimer’s Disease
Several studies suggest that there may be an interdependent relationship between OSA and Alzheimer’s disease, as they are particularly common in older populations and frequently coexist. One analysis found that about 50 percent of Alzheimer’s patients experience OSA after their initial diagnosis.
Depression
Both OSA and depression have many of the same symptoms: restlessness, fatigue, poor concentration, and more. While the exact relationship between depression and OSA remains unclear, studies have found that the prevalence of depression is higher in patients with OSA as compared to the general population.
Poor breathing and sleep can impact nearly every area of your body, including your mental, physical, and emotional health.
Effects on Your Health
Beyond long-term conditions that can affect your health, OSA can also harm many of the processes that take place in your body, including your respiratory, digestive, immune, nervous, and reproductive systems. Here’s how.
Respiratory System
Sleep apnea deprives the body of oxygen while you sleep, which can result in crippling results such as worsened symptoms of asthma and chronic obstructive pulmonary disease (COPD). OSA and COPD overlap so often that there’s a name for the phenomenon: overlap syndrome. Many individuals with OSA also find themselves out of breath more often, as well as having a harder time exercising than usual.
Digestive System
Those with sleep apnea are at a higher risk of having fatty liver disease, liver scarring, and high levels of liver enzymes. OSA can also worsen acid reflux (heartburn), leading to more interruptions to your sleep. OSA is associated with an increased risk of developing Barrett’s esophagus, a precancerous condition that may lead to esophageal cancer.
Immune System
A lack of sleep caused by OSA can weaken your immune system. When your body doesn’t get the rest it needs to repair itself throughout the night, it has a hard time creating antibodies that help fight off infection. As a result, you and your partner may get sick a lot more often than you’re used to. A population-based study found an increased risk of pneumonia for individuals with OSA.
Nervous System
OSA causes your body to force itself awake in order to breathe, resulting in the overactivation of your sympathetic nervous system. This part of the brain is responsible for your stress response. Not only can this lead to prolonged feelings of stress and anxiety, but research also suggests it may even impact your visuospatial functioning. Know what that means? You’re more likely to misjudge distances, bump into things, and get in a car accident. Research indicates a relationship between OSA and various sight-threatening eye conditions.
Reproductive System
If you think it’s possible that your husband has sleep apnea, this is one area to pay particular attention to. Researchers from Sleep studying mice found that chronic, high-frequency sleep apnea is linked to reduced male fertility, erectile dysfunction, and lower libidos. Although sleep apnea affects both men and women, in men, it could contribute to their ability to have children.
Long-Term Implications
The longer obstructive sleep apnea goes undiagnosed and untreated, the more time it has to become more severe and exacerbate symptoms that can affect every area of the body. If you feel that your partner may have sleep apnea, it’s important to have a conversation with them as soon as possible so they can reach out to a medical professional and get the treatment they need.

Women Can Have Sleep Apnea, Too
You may have heard all about women complaining about snoring from their husbands. Along those lines, the media makes it seem like only men experience snoring and sleep apnea. This couldn’t be further from the truth. While men are more likely to have OSA, women also suffer from the disorder. As people age, the disparity between sexes declines: Both men and women between the ages of 50 and 59 show a steep increase in sleep apnea.
It’s essential to be aware of snoring and OSA in women—particularly because they may be even less likely to realize they snore or have a breathing disorder. In a study from the Journal of Clinical Sleep Medicine, over one-third (nearly 37 percent) of the women who reported themselves as non-snorers turned out to have severe or very severe snoring intensity. In contrast, only 11.7 percent of men had this discrepancy. As a result, many women may be underdiagnosed and undertreated for the disorder. For menopausal women, OSA symptoms are often attributed to menopause, which can cause a further delay in an OSA diagnosis.
If you notice your wife snoring and think she may have OSA, it’s just as important for her to reach out to a medical professional for help. Along those lines, it’s also essential to help her watch for the lesser-known signs of OSA—such as insomnia, sleep fragmentation, depression, fatigue, or morning headaches—that may be more common in women than men.
Tips on Talking to Your Partner about Treatment
Talking to your partner about sleep apnea can be tricky. Between heightened emotions, sleeplessness, and tension over your sleeping arrangements, it can be challenging to get your point across calmly and clearly.
Before sitting down with your partner about the quality of their sleep, take the time to come up with a few ways you can help yourself get better sleep despite their snoring. For example, wearing earplugs, listening to a white noise machine, changing your sleep position, and sleeping in a separate room could all help you get great sleep before speaking to your partner about their nighttime rumbling.
Here are a few additional tips that can also help you express why treatment is so important for your partner.
Emphasize the Health Dangers, Not the Annoyance or Inconvenience
We know just how aggravating sleep deprivation can be—especially when it’s 2 am and you’re lying wide awake next to someone who seems to be sleeping just fine, however loud it may be. However, when it comes to talking to your partner about their snoring and possible sleep apnea, it’s important not to focus on your own annoyance or inconvenience.
Instead, pay close attention to expressing why sleep apnea is a risk to their health. Be honest about why you’re concerned about their symptoms, and explain how getting help would benefit them. Rather than responding defensively, your partner will be more likely to listen openly and look into treatment options if they realize just how serious their snoring may be.
Explain That They’ll Get Much Better Sleep
On top of the serious health concerns associated with OSA, it also impacts how they feel throughout the day. Explain just how much sleep apnea affects their sleep quality, and be sure to point out the benefits of treatment in their everyday life.
The following are just a few of the positive results they could experience by addressing their sleep apnea and getting better sleep:
- Improved immune function and less sickness
- Weight loss and an easier time staying at a healthy weight
- Reduced stress
- Better mood
- Clearer thinking
- Improved job and school performance
- Better interpersonal relationships
As you speak with your partner about their snoring, it’s important to focus on them and their experiences. Ask them how their snoring makes them feel. At the end of the day, they’ll feel a lot more comfortable talking to you about it if they don’t feel attacked or ashamed by how much their snoring has affected you.
If you think your partner has sleep apnea, it’s essential that you reach out to a dentist and another medical professional as soon as possible. Not only is the sleep disorder associated with debilitating daytime symptoms, but it may also contribute to serious health concerns. Most importantly, these professionals will be able to screen and diagnose the sleep disorder, as well as walk your partner through the best treatment options available based on the severity of their sleep apnea, lifestyle, and goals.
If you still have questions about sleep apnea, visit our website at vivos.com to learn more.
References
References Here
The statements made on this website are for educational purposes and include articles, educational materials, and research on various topics within the Sleep and Dental industries and are not the views of, or are in connection with Vivos Therapeutics and/or its regulated products. The statements are not intended to accompany any required product labeling for a regulated product. Neither are such statements intended to introduce a new indication, patient population, alter the directions for use, or otherwise change or supplement any required labeling for a regulated product.

